Researchers
For more information, visit the CDEHA website at https://cdeha.stanford.edu
Overview
CDEHA builds upon and integrates work across multiple disciplines at Stanford in population studies, health economics, economics of retirement and medical technology assessment; and across multiple disciplines including statistics, econometrics, epidemiology, population biology and demography.
Program areas within CDEHA include health disparities; the economics of retirement and demographic change; international population studies; the effects of medical technology on costs, outcomes and well-being of the elderly; and longitudinal and cohort studies of medical care, costs, and health and economic outcomes in the United States and other countries. The center also encourages cross-disciplinary collaborations and recruits promising trainees and junior faculty to conduct research in this area.
Video of Jay Bhattacharya discusses health and aging
Need for this research
The United States and many other nations are experiencing a rapid increase in their elderly populations, prompting questions about future healthcare needs, how to finance care, and the nature of retirement. To address these issues, CDEHA promotes the study of trends in demography, economics, health, and health care, and the effects of these trends on the well-being of the elderly.
Funding provided by the National Institute on Aging (NIA)
Aims of the Center
1. To promote the conduct of longitudinal and cohort studies of medical care, costs, demographics, and health and economic outcomes of older populations, in the United States and other countries.
2. To promote the application of demographic techniques, including biodemography, to understand changes in survival, health, and well-being among the elderly over time.
3. To promote the study the effects of medical technology and health care decisions on costs, health outcomes, and well-being of the elderly.
4. To promote and enhance research in the demography and economics of aging at Stanford and in collaborating institutions.
Recent Pilot Projects:
This study aims to assess the extent to which wealth accurately proxies health status in low- and middle-income countries. Specifically it is testing the hypothesis that absolute wealth is much more important for health than wealth inequalities or relative wealth. The researchers have collected 150+ DHS surveys with suitable information on wealth and health outcomes, and have finalized and validated a harmonized wealth index that allows for measuring absolute and relative wealth gradients. They validated the index against education status, which does not enter into the creation of the index, and created harmonized and general measures of health, including malnutrition, stunting, and infant mortality in the household. They are now preparing to analyze the strength and stability of the relationship between wealth (measured as either absolute or relative) and health outcome.
Adapting the Future Elderly Model to Japan, Karen Eggleston [2014-2015]
This project adapts the Future Elderly Model (FEM), a demographic and economic Markov microsimulation model that projects the health conditions and functional status of an elderly population, to the Japanese population. The model starts with a “snap-shot” of the middle-aged and elderly Japanese population in 2010 and then projects risk of developing 19 chronic conditions, health care utilization, annual medical expenditures, and mortality. The researchers have received and analyzed the basic Japanese Study of Aging and Retirement (JSTAR) data; developed appropriate estimates of conditional mortality for the relevant diseases for the Japanese elderly; constructed a micro-simulation model; and used the 2007-2013 claims data for over 84,000 Japanese aged 40 to 70 to predict the medical spending associated with different constellations of medical conditions. The researchers will now look at how spending conditional on given co-morbidities differs by age group, and develop projections appropriate for the above-70 population. They have completed a preliminary integration of medical spending projections by age and health status into the FEM built from multiple waves of the JSTAR to estimate the health status transition matrix.
This project explores the first period of decline in infant mortality in the U.S. and provide estimates of the independent and combined effects of clean water and effective sewerage systems on infant mortality. Our case is Massachusetts, 1880-1915, when state authorities developed a sewerage and water district for municipalities in the Boston Greater Metropolitan area. We find that the two interventions were complementary and together accounted for approximately 44 percent of the total decline in log infant mortality among treated municipalities during the 35 years considered. Considerable research has documented the importance of clean water interventions for improvement in population health, but there is less evidence on the importance of sewerage systems. Our findings are directly relevant to urbanization in the developing world and suggest that a dual-pronged approach of safe water and sewerage is important to improving infant and early child survival.
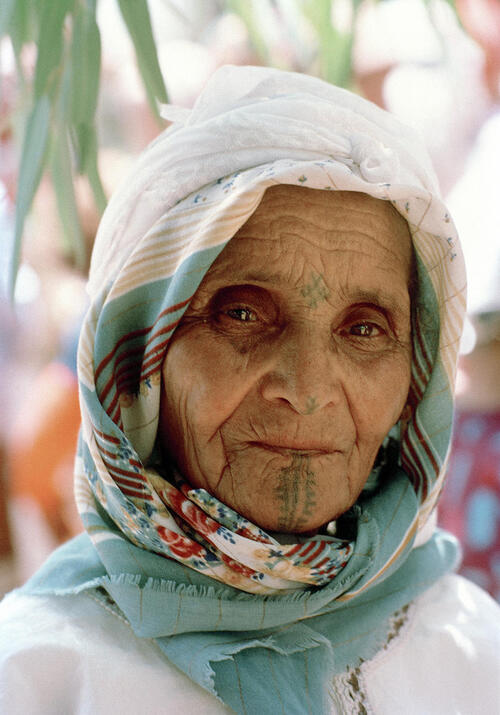
Chronic Disease, Disability, and Medical Costs among Older Adults in India, Sanjay Basu [2013-2014]
The researchers conducted a series of studies using nationally-representative data from the recent WHO Study on Global Aging and Adult Health (SAGE) to identify the relationship between NCD-related disability among adults over 50 years of age in India and healthcare utilization and costs. The study to date has found that older rural women were disproportionately affected by non-diagnosed NCDs, with high out of pocket healthcare expenditures increasing the probability of remaining symptomatic from NCDs. The study also investigated disparities in NCD disability across the income gradient and found that rural and lower-income populations were more likely to have NCDs that were not captured by typical surveys that only asked for formally-diagnosed NCDs; rather, the SAGE study, by including validated symptom scales to diagnose several NCDs, revealed a high prevalence of undiagnosed NCDs among the poor, and a higher prevalence of several NCDs among these lower-income groups.

Effect of Social Isolation and Loneliness on Health Care Utilization, Jonathan Shaw [2013-2014]
The researchers assessed the effect of social isolation and loneliness on healthcare utilization (costs and frequency of care) using longitudinal survey data from the Health and Retirement Survey (HRS) linked to Medicare administrative claims data. This study provides the first representative picture of the correlation social isolation and loneliness have with total Medicare costs. Additional project funding was obtained from the AARP Public Policy Institute. Analysis and sub-analyses are now largely complete and the initial findings have been presented internally to researchers within Stanford and AARP Public Policy Institute; final results are being prepared for submission for peer-reviewed publication and the release of findings may be coordinated with the AARP Public Policy Institute to convene a research and policy meeting around the topic of social isolation and health.
The researchers are developing prior work on the temporal, spatial and socioeconomic variation in US mortality for males and females. To achieve these goals they will assemble a data set of time series of mortality rates by age, cause and sex, and assemble a data set of relevant socio-economic and environmental variables for all US counties starting in 1970. Data set assembly now nearly complete, code for county-level comparisons of variance written and tested, and a new focus on male-female comparisons, so far mainly done with international data. International analyses are the first to causally demonstrate that changes in causes of death that are strongly influenced by tobacco use are responsible for the change in the female-male difference in life expectancy. These results are one of the few that demonstrate, at whole-country population level, the impact of a single public health change. Further, the study makes novel use of high-quality demographic data, cause-of-death data curated by WHO, and decompositions of mortality rates that have rarely been used in epidemiologic or public health literature.

Readmissions and Chronic Disease in the Elderly, Kathryn McDonald [2012-2013]
This study aimed to expand knowledge regarding chronic disease and readmissions in the elderly The researchers conducted a retrospective analysis of California Office of Statewide Health Planning and Development Patient Discharge Data, 2000-2009, which includes all adults age 18 and older with a non-federal acute care hospital discharge (n= 29,009,966 discharges). We identified 7- and 30-day all cause readmissions (ACR) and potentially preventable readmissions (PPR), and then analyzed relationships between index and readmission hospitalizations for each metric. They found that in the eligible samples, the 30-day ACR and PPR rates were 10.0% and 5.6% respectively. Index admissions for Heart Failure had the most 30-day ACRs and highest readmission rate (103,591, 19.8%) among medical APR-DRGs, while Other Vascular procedures had the highest rate (14,635, 14.6%) among surgical APR-DRGs. Overall, relatedness of readmissions did not differ for 7- vs. 30-day ACRs. The PPR algorithm captured fewer unrelated readmissions than did the ACR for surgical but not medical APR-DRGs. Unrelated readmission captured by PPR included both acute and chronic conditions, in particular ambulatory care sensitive conditions. This study demonstrates that the concept of relatedness is similar to, but not identical to “potentially preventable” as determined by the PPR metric. Both the ACR and PPR provide a unique perspective on readmissions and can be useful across applications. The reasons for readmission captured by both metrics can provide guidance for potentially impactful interventions. Three manuscripts related to the project have been published by Health Services Research, American Journal of Medical Quality, and the International Journal for Quality in Health Care, and a fourth manuscript is under review.
Pilot Project Work Products (2013 - Present)
Since 2013, CDEHA's support of pilot projects has contributed to the publication of 23 peer-reviewed articles, one NBER working paper, and one book chapter in addition to 15 presentations and 16 meeting abstracts. During this time, 12 grants and awards resulting from CDEHA pilots were in active status. Furthermore, eight papers related to CDEHA pilot projects are currently under review and eight manuscripts are in preparation. See a full list of CDEHA pilot project publications.
Recent Events
"Informing Health Care System Innovation at Both Ends of Life: Improving Care in Pediatrics and Geriatrics"
Lee Sanders; Mary Goldstein
October 1, 2014
"Who Enrolls in Medicare Advantage? Evidence from the Health and Retirement Study"
Kate Bundorf
October 29, 2014
"The Weaker Sex? Vulnerable Men, Resilient Women, and Variations in Sex Differences in Mortality Since 1900"
Karen Eggleston
January 7, 2015
"Changing Choice Architecture to Improve End-of-Life Care"
Scott Halpern
January 28, 2015
"Early Fertility Decline and Sex Imbalance in Rural China"
Grant Miller
February 11, 2015
"Age and Trying Out New Ideas"
Jay Bhattacharya
February 25, 2015